Background: In phase one of the development of the PROFID risk prediction model we analysed 19 datasets from Europe, Israel and the US, based on a collection of existing highly phenotyped data with the largest number of post-MI patients (~225,000 observations). LVEF was found to be a poor predictor of SCD. Consideration of the large variety of additional variables (demographics, clinical parameters, medication, ECG, biomarkers, echocardiograph etc.) also did not improve predictive performance. In phase two of the PROFID analysis, we therefore updated the prediction model with inclusion of cardiac magnetic resonance (CMR) variables.
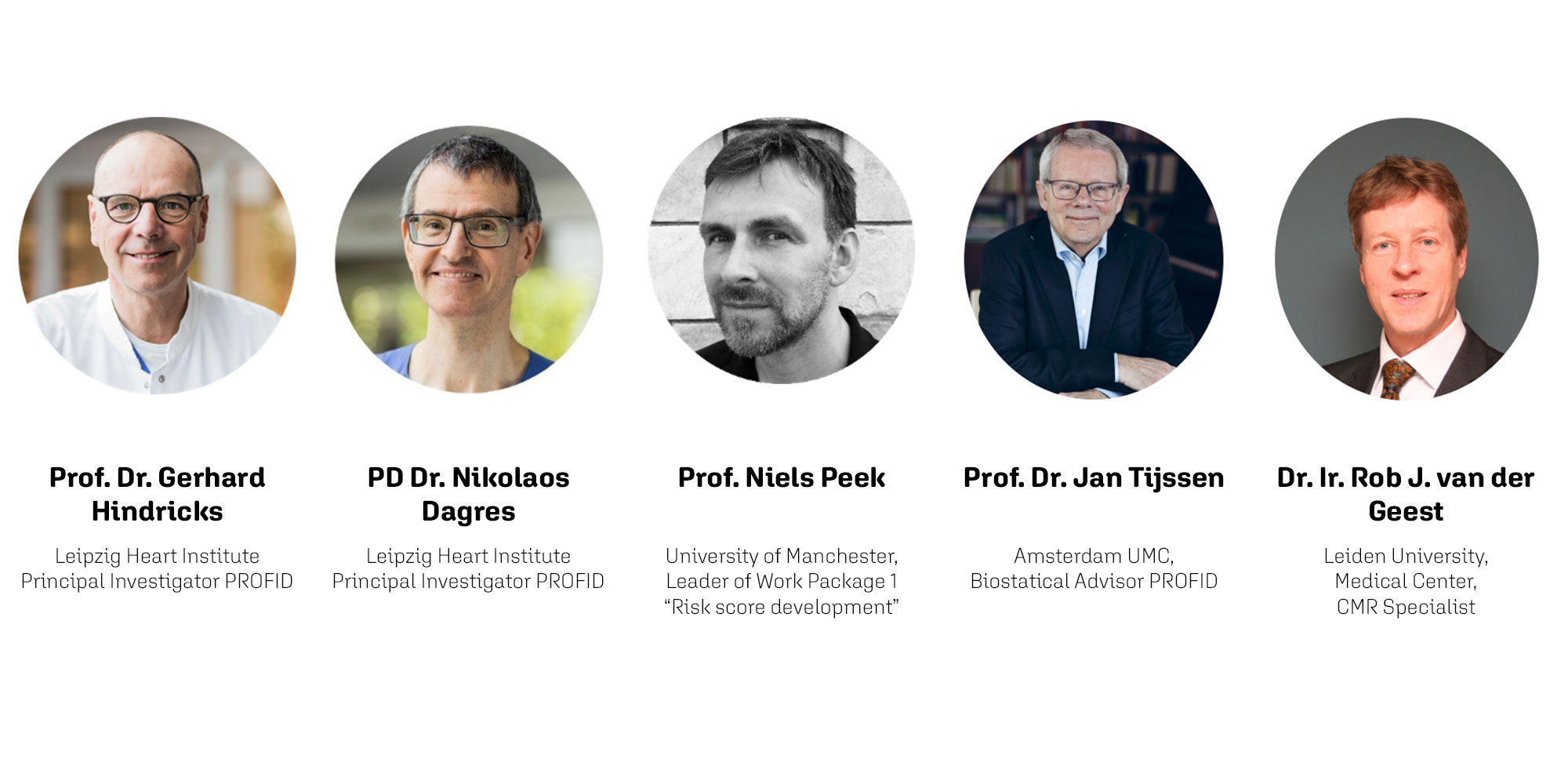
Why was the re-analysis of 7 CMR data sets necessary?
Gerhard Hindricks: “Previous studies have indicated a predictive value of fibrosis detection by CMR for the assessment of SCD risk. However, there is significant heterogeneity in the definition of scar and grey zone in the literature that limits the interpretation of study findings. In order to unmask the true potential of this data for SCD prediction, we reanalysed 7 datasets from Europe and the United States comprising patients with previous MI (regardless of LVEF), or ischemic cardiomyopathy with LVEF<50%, in whom CMR had been performed at least 40 days after MI. With ~2.100 patients, we are presenting the largest cohort of CMR data analysed for predicting the risk of SCD. An extensive re-evaluation of the CMR studies was performed in order to achieve consistent CMR measurements of scar size and grey zone size across all 7 datasets, to reduce measurement heterogeneity and compare different previously applied thresholds for core scar and grey zone quantification.”
Please give us a short overview about the work that has been done by the Manchester Team during the re-analysis of the CMR studies.
Niels Peek: “Using the largest collection of CMR data in this context to-date, we have examined if core scar and grey zone add significant value for predicting sudden cardiac death over LVEF alone, while adjusting for death from other causes. This required that several CMR datasets were re-evaluated, which has been done by Rob van der Geest, to ensure consistency in the manner in which core scar and grey zone were estimated from the CMR images.
We liaised with CMR data providers to ensure that all data transfers and analyses were conducted in line with jurisdictional, legal, and ethical stipulations. Fortunately, all data providers were extremely collaborative and helped to re-evaluate the respective CMR datasets within the short timeframe available. Remote data access procedures were implemented following on-site manual annotation and segmentation, allowing Rob to estimate relevant CMR parameters. All extracted parameters were subsequently securely transferred to the University of Manchester for further analysis.
In the statistical analysis we then considered several combinations of core scar and grey zone classifications, to find the best performing classification across the 7 CMR datasets, to risk stratify ICD implantation in patients with reduced LVEF.”
Rob, you joined the PROFID Team at the end of 2021. What was your task and what were your expectations?
Rob van der Geest: “My task was to carry out a re-analysis of the multi-center late-enhancement CMR datasets. The main objective was to standardize the way scar core and scar grey zone are quantified from the CMR data such that the results from the different cohorts can be compared.”
Why was it so important to include your statistical experience in the re-analysis?
Jan Tijssen: “My statistical experience is deeply rooted with cardiovascular research. For almost all of my career, I have worked on clinical research within the Department of Cardiology together scientifically active clinicians, first in Rotterdam and later in Amsterdam. Over the years, I have learned to converse with clinical cardiologists about study design, statistical analyses, and the interpretation of the findings of clinical studies, all within the domain of clinical cardiology and cardiovascular disease. Over the last 5 years, I have expanded my experience in clinical research from the perspective of a (statistical) editor and reviewer of a major cardiovascular journal. Taken together, I hope can use my statistical experience to tailor the statistical analyses of PROFID to the need for clinically applicable new knowledge about the usefulness of ICD implantation in post-MI patients in current clinical practice.”
What was particularly challenging about the re-analysis of these data?
Rob van der Geest: “The main challenge was to create a setup to automate the data analysis as much as possible, including facilities for time-efficient visual quality checks and manual contour editing whenever needed. The CMR data was previously analysed by the data providers using different software packages and extracting the contour information from the existing result files was one of the required steps. In the end we were able to automate the scar analysis for the patient cohorts in a fully automated manner using multiple methods for scar core and grey zone segmentation.”
What was the biggest challenge for you and your team? What issues did you have to face and how did you deal with them?
Niels Peek: “A key challenge was the fact that there was a very short timeframe to conduct the CMR re-evaluation and subsequent statistical analysis. Furthermore, some heterogeneity between estimated core scar and grey zone values unexpectedly persisted after the CMR re-evaluation. For the Manchester team a further challenge was to harmonise the datasets, as they came with very different shapes and sizes, and not all had CMR parameters in grams. Finally, the event rate (sudden cardiac death / ICD shocks) was a challenge for the statistical analysis because the CMR datasets are smaller than the clinical datasets that we analysed in Phase 1.”
Which new insights have you gained during the creation of the PROFID risk prediction model?
Nikolaos Dagres: “The phase 1 analysis on ICD and non-ICD datasets provided two main findings; LVEF had moderate predictive performance for the risk of SCD in patients with previous MI or ischemic cardiomyopathy with reduced LVEF <50% and the consideration of 76 further candidate predictors that are available in clinical routine did not improve the predictive performance.
The 7 CMR datasets used in phase 2 of the analysis represent the largest multi-centre collection of end-point adjudicated CMR data. Considering several recent reports on the value of CMR, the inclusion of such a large collection was decisive.
Furthermore, it has once again been shown how incredibly important good partnerships are. Without the support of all those experts involved, the analysis would never have been possible.”
How would you evaluate the results that have been achieved during the re-analysis?
Jan Tijssen: “The journey with the PROFID team has been exciting with many expected and some unexpected turns. Gerd, Nikos and the Manchester team have collated a unique series of databases with baseline characteristics and outcomes in various populations of patients with a recent myocardial infarction, with left ventricular ejection fraction and ICD implantation as the central determinants of the risk of sudden cardiac death. The use of CMR data has opened a novel and promising avenue in risk prediction for sudden cardiac death in patients with a recent myocardial infarction.”
Why are these results so important and how do they influence the PROFID project?
Gerhard Hindricks: “This has been an exciting but also very challenging task for the last 2.5 years and builds the basis for the whole project. Now it is time to proceed to the next decisive phase of the project, which is the conduction of the PROFID trials. For this, we need to look further at the results of the data analysis, discuss their implications and finalize the setup of the trials so that they bring us as close as possible to the aim of PROFID: an optimal decision-making on primary prevention ICD implantation after myocardial infarction.”
What are the next steps within the PROFID project and what do you expect to achieve?
Nikolaos Dagres: “The incredibly complex and extensive process of data analysis is finalized, thanks to the fantastic support from our amazing partners. We are now going to implement the results in the upcoming randomised multi-centre clinical trials. Furthermore those results are going to be presented as a late breaker at the next ESC Congress in August 2022 in Barcelona, which we are very proud of.”